Abstract
Background
As bariatric surgery becomes ever more popular, so does body-contouring surgery to eliminate excess skin after radical weight loss. To date, the literature has described a number of risk factors affecting the postoperative outcome. Our study aimed to define those factors more closely, focusing on abdominoplasty (“tummy tuck”) patients who suffered intra- and postoperative complications.
Methods
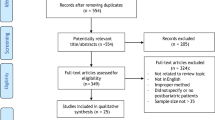
The study collective included 205 patients over 5 years (2001–2006) who underwent dermolipectomy at our department. The mean follow-up was 5.94 years. Every abdominoplasty was performed under general anesthesia with intraoperative one-dose antibiotic. The analysis included a complete review of all medical records. Statistical analysis was performed with the R-2.5.0 Software for Windows.
Results
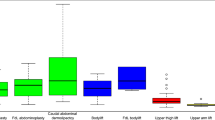
The overall rate for major complications that required operative revision and/or antibiotics was 10.2 %, including 2.9 % cases of infections. Forty-one percent had minor complications, such as seromas, hematomas, wound healing problems, and wound dehiscences. The logistic regression models demonstrated that smoking combined with the age, a BMI higher than 30 kg/m2, and the amount of removed tissue (measured in g) lead to significantly more wound healing problems in nearly all age groups. The probability of infections correlated with later drain removal.
Conclusions
Regardless of the amount of tissue removed, no main risk factor for complications could be identified. A complication-free course and good outcome can be best achieved with careful patient selection and preoperative planning.










Similar content being viewed by others
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA J Am Med Assoc. 2004;292:1724–37.
Vastine VL, Morgan RF, Williams GS, et al. Wound complications of abdominoplasty in obese patients. Ann Plast Surg. 1999;42:34–9.
Arthurs ZM, Cuadrado D, Sohn V, et al. Post-bariatric panniculectomy: pre-panniculectomy body mass index impacts the complication profile. Am J Surg. 2007;193:567–70. discussion 570.
Neaman KC, Hansen JE. Analysis of complications from abdominoplasty: a review of 206 cases at a university hospital. Ann Plast Surg. 2007;58:292–8.
Greco 3rd JA, Castaldo ET, Nanney LB, et al. The effect of weight loss surgery and body mass index on wound complications after abdominal contouring operations. Ann Plast Surg. 2008;61:235–42.
Au K, Hazard 3rd SW, Dyer A-M, et al. Correlation of complications of body contouring surgery with increasing body mass index. Aesthetic Surg J Am Soc Aesthetic Plast Surg. 2008;28:425–9.
De Kerviler S, Hüsler R, Banic A, et al. Body contouring surgery following bariatric surgery and dietetically induced massive weight reduction: a risk analysis. Obes Surg. 2009;19:553–9.
Hensel JM, Lehman Jr JA, Tantri MP, et al. An outcomes analysis and satisfaction survey of 199 consecutive abdominoplasties. Ann Plast Surg. 2001;46:357–63.
Rogliani M, Labardi L, Silvi E, et al. Smokers: risks and complications in abdominal dermolipectomy. Aesthetic Plast Surg. 2006;30:422–4. discussion 425.
Gravante G, Araco A, Sorge R, et al. Wound infections in post-bariatric patients undergoing body contouring abdominoplasty: the role of smoking. Obes Surg. 2007;17:1325–31.
Agha-Mohammadi S, Hurwitz DJ. Potential impacts of nutritional deficiency of postbariatric patients on body contouring surgery. Plast Reconstr Surg. 2008;122:1901–14.
Grazer FM, Goldwyn RM. Abdominoplasty assessed by survey, with emphasis on complications. Plast Reconstr Surg. 1977;59:513–7.
Pitanguy I. Abdominal lipectomy. Clin Plast Surg. 1975;2:401–10.
Hester Jr TR, Baird W, Bostwick 3rd J, et al. Abdominoplasty combined with other major surgical procedures: safe or sorry? Plast Reconstr Surg. 1989;83:997–1004.
Smith MM, Hovsepian RV, Markarian MK, et al. Continuous-infusion local anesthetic pain pump use and seroma formation with abdominal procedures: is there a correlation? Plast Reconstr Surg. 2008;122:1425–30.
Khan UD. Risk of seroma with simultaneous liposuction and abdominoplasty and the role of progressive tension sutures. Aesthetic Plast Surg. 2008;32:93–9. discussion 100.
Araco A, Gravante G, Sorge R, et al. Wound infections in aesthetic abdominoplasties: the role of smoking. Plast. Reconstr. Surg. 2008;121:305e–310e.
Brink RR, Beck JB, Anderson CM, et al. Abdominoplasty with direct resection of deep fat. Plast Reconstr Surg. 2009;123:1597–603.
Araco A, Gravante G, Araco F, et al. Postoperative seromas after abdominoplasty: a retrospective analysis of 494 patients and possible risk factors. Plast. Reconstr. Surg. 2009;123:158e–159e.
Araco A, Sorge R, Overton J, et al. Postbariatric patients undergoing body-contouring abdominoplasty: two techniques to raise the flap and their influence on postoperative complications. Ann Plast Surg. 2009;62:613–7.
Matarasso A, Swift RW, Rankin M. Abdominoplasty and abdominal contour surgery: a national plastic surgery survey. Plast Reconstr Surg. 2006;117:1797–808.
Manassa EH, Hertl CH, Olbrisch R-R. Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plast Reconstr Surg. 2003;111:2082–7. discussion 2088–2089.
Nemerofsky RB, Oliak DA, Capella JF. Body lift: an account of 200 consecutive cases in the massive weight loss patient. Plast Reconstr Surg. 2006;117:414–30.
Van der Beek ESJ, van der Molen AM, van Ramshorst B. Complications after body contouring surgery in post-bariatric patients: the importance of a stable weight close to normal. Obes Facts. 2011;4:61–6.
Dixon AJ, Dixon MP, Dixon JB. Prospective study of skin surgery in patients with and without known diabetes. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2009;35:1035–40.
Andrades P, Prado A, Danilla S, et al. Progressive tension sutures in the prevention of postabdominoplasty seroma: a prospective, randomized, double-blind clinical trial. Plast Reconstr Surg. 2007;120:935–46. discussion 947–951.
Warner JP, Gutowski KA. Abdominoplasty with progressive tension closure using a barbed suture technique. Aesthetic Surg J Am Soc Aesthetic Plast Surg. 2009;29:221–5.
Pollock TA, Pollock H. Progressive tension sutures in abdominoplasty: a review of 597 consecutive cases. Aesthetic Surg J Am Soc Aesthetic Plast Surg. 2012;32:729–42.
Fang RC, Lin SJ, Mustoe TA. Abdominoplasty flap elevation in a more superficial plane: decreasing the need for drains. Plast Reconstr Surg. 2010;125:677–82.
Di Martino M, Nahas FX, Barbosa MVJ, et al. Seroma in lipoabdominoplasty and abdominoplasty: a comparative study using ultrasound. Plast Reconstr Surg. 2010;126:1742–51.
Kim J, Stevenson TR. Abdominoplasty, liposuction of the flanks, and obesity: analyzing risk factors for seroma formation. Plast Reconstr Surg. 2006;117:773–9. discussion 780–781.
Swanson E. Prospective photographic measurement study of 196 cases of breast augmentation, mastopexy, augmentation/mastopexy, and breast reduction. Plast. Reconstr. Surg. 2013;131:802e–19e.
Najera RM, Asheld W, Sayeed SM, et al. Comparison of seroma formation following abdominoplasty with or without liposuction. Plast Reconstr Surg. 2011;127:417–22.
Van Uchelen JH, Werker PM, Kon M. Complications of abdominoplasty in 86 patients. Plast Reconstr Surg. 2001;107:1869–73.
Souto LRM, Chaim EA, Barbosa RC, et al. Increased intraoperative bleeding in patients undergoing abdominoplasty after gastroplasty is not due to coagulopathy. Aesthetic Plast Surg. 2012;36:1283–91.
Stovner LJ, Hagen K. Hypertension-associated hypalgesia: a clue to the comorbidity of headache and other pain disorders. Acta Neurol Scand Suppl. 2009;46–50.
Fecho K, Miller NR, Merritt SA, et al. Acute and persistent postoperative pain after breast surgery. Pain Med Malden Mass. 2009;10:708–15.
Campbell TS, Hughes JW, Girdler SS, et al. Relationship of ethnicity, gender, and ambulatory blood pressure to pain sensitivity: effects of individualized pain rating scales. J Pain Off J Am Pain Soc. 2004;5:183–91.
Acknowledgments
We agreed to the submitted version of the paper and bear responsibility for it, that all who have been acknowledged as contributors or as providers of personal communications have agreed to their inclusion, that the material is original, and that it has been neither published elsewhere nor submitted for publication simultaneously. We accepted that the paper will not be published elsewhere in the same or similar form, in English or in any other language, without written consent of the copyright holder.
Disclosure
The authors have no financial disclosures to declare.
Conflict of Interest
All named authors declare no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human and Animal Rights
The protocol of this analysis was approved by the Institutional Review Board of the Medical University of Graz and was in accordance with the Helsinki Declaration of 1975 (revised 2000).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parvizi, D., Friedl, H., Wurzer, P. et al. A Multiple Regression Analysis of Postoperative Complications After Body-Contouring Surgery: a Retrospective Analysis of 205 Patients. OBES SURG 25, 1482–1490 (2015). https://doi.org/10.1007/s11695-014-1559-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1559-5